CONGRESSIONAL TESTIMONY
Testimony before
Committee on Health, Education, Labor and Pensions (HELP)
United States Senate
May 2, 2024
Yolanda Lawson, MD, F.A.C.O.G
124th President of the National Medical Association
Greetings Chairman Sanders, Ranking Member Bill Cassidy, M.D., and Members of the Committee.
Thank you for the opportunity to appear before the committee to discuss this critical issue: addressing the shortage of minority healthcare professionals.
My name is Yolanda Lawson, M.D. I am testifying today as an OB-GYN practicing in Dallas, Texas, and as the President of the National Medical Association, the largest and oldest national organization representing the interests of more than 50,000 African American physicians and the patients they serve.
I am the founder of MadeWell OBGYN in Dallas and MadeWell Woman, a birthing center. I am currently the Executive Medical Director, Maternal Infant Health at HealthCare Services Corp.
As a physician, my first duty is to the health of my patients. As NMA president, my first priority is to represent the needs of Black physicians and Black communities in this country.
The sad fact is: Patients who are African American, as well as other people of color, are not as healthy as their white (non-minority counterparts.) And these disparities have existed since federal recordkeeping began.
The COVID-19 pandemic brought this issue to the forefront. In 2020, the entire nation watched in horror as members of the Black community accounted for a disproportionate number of COVID-19 deaths.
That was an extraordinary situation but reflected a chronic issue. Black people are disproportionately affected by every major chronic disease (excluding those with a genetic basis). They are 2.2 more likely to have diabetes. According to the CDC Black infants 2.4 times the mortality of White infants. African-Americans have the highest mortality rates of any racial or ethnic group for all cancers combined and most major cancers. Black people are more likely to die of heart disease than any other group. Black women are 60% more likely to have high blood pressure compared to White women.
Other disparities include “higher uninsured rates, being more likely to go without care due to cost, and worse reported health status. The life expectancy of Black people is nearly five years shorter compared to White people (72.8 years vs. 77.5 years).”
Even more disturbing are disparities in maternal health. Black women continue to experience disproportionately high rates of maternal morbidity and mortality compared to white counterparts. The Centers for Disease Control and Prevention (CDC) reports that Black women are three to four times more likely to die from pregnancy-related complications than white women.
MATERNAL HEALTH DISPARITIES: A PERSISTENT CHALLENGE
Maternal health disparities persist as a pressing public health challenge in the United States. Despite advances in medical technology and healthcare delivery, Black women continue to experience disproportionately high rates of maternal morbidity and mortality compared to their white counterparts. The Centers for Disease Control and Prevention (CDC) reports that Black women are three to four times more likely to die from pregnancy-related complications than white women. These disparities are not solely attributable to socioeconomic factors but are deeply rooted in systemic racism, implicit bias, and unequal access to quality healthcare.
This is not just a matter of equity. The commitment to safe birthing processes and positive health outcomes affects everyone, not just mothers. When there are more sick people, that creates a bigger burden on our healthcare system, less productivity for the affected workforce, and higher medical costs that ultimately, we all pay for, whether through higher health insurance premiums or tax dollars for Medicare and Medicaid. In 2019, it was noted that the impacts of maternal morbidity cost the United States $32.3 billion.
To address this problem, we must understand why it’s happening. These disparities are not attributable solely to socioeconomic factors. Nor is there a genetic or biologic basis. They are deeply rooted in a myriad of factors that include systemic racism, implicit bias, and unequal access to quality healthcare. But one key factor, which I’d like to address in depth, is the shortage of Black physicians.
MORE BLACK PROVIDERS
Research consistently demonstrates that patients from racial and ethnic minority backgrounds experience better health outcomes when treated by healthcare providers who share their racial and ethnic backgrounds. In short, patients can have better outcomes when their doctors look like them.
Yet Black doctors remain vastly underrepresented relative to their proportion of the U.S. population. Despite long-standing efforts to increase minority representation in our physician workforce, gains have been minimal. African American and Black people represent only 5.7% of physicians – which means they are grossly underrepresented relative to the roughly 13.6% of Americans who are Black.
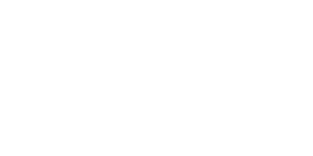
Physicians, of course, are only part of the healthcare workforce. Recently, the NMA’s Annual Colloquium convened the presidents of all the major organizations of Black healthcare providers, including Black nurses, Black pharmacists, Black registered dieticians, and Black physical therapists, Black Dentists and Black Psychologists. We all agreed: Ensuring the future of a diverse workforce is critical to ending healthcare disparities.
Why is representation so important? Why do Black patients seem to do better when they see Black physicians?
One reason is that Black physicians and healthcare providers are more likely to understand the unique challenges that influence Black patients’ health outcomes. Also, Black patients are more likely to trust the advice of a Black physician or provider and comply with the physician’s recommendations. Sociocultural understanding and improved communication can lead to better quality of care. Studies indicate that black infants are 3x more likely to die than non-Hispanic white infants, however that number decreases by half when they are seen by a Black doctor. Similarly, cardiovascular deaths in Black men are reduced by 19% when they are seen by a Black physician.
Trust is critical in creating positive health outcomes and there is a legacy of distrust in our community. This history of distrust is understandable given the history of healthcare delivery and research in the United States. The Tuskegee syphilis study is widely recognized as one key reason for this mistrust. However, studies suggest that the history of medical and research abuse of African Americans goes well beyond Tuskegee.
Distrust has so many repercussions and costs. Despite mandates by the federal government to ensure inclusion of women and minorities in all federally funded research, African Americans continue to participate less frequently than Whites. Lower participation rates among African Americans have been reported across various study types (e.g., controlled clinical treatment trials, intervention trials, as well as studies on various disease conditions, including AIDS, Alzheimer’s disease, prostate cancer and other malignancies, stroke, and cardiovascular disease). Black people don’t enroll in research studies because of that legacy of distrust. The presence of more Black physicians could begin to repair some of that distrust.
Black physicians and healthcare providers can advocate for equitable healthcare policies and practices within the healthcare system.
UNDERSTANDING BARRIERS
Several challenges persist for young Black people who aspire to become physicians:
Structural barriers – including limited access to medical school education, financial constraints, pervasive discrimination within academic and healthcare settings – all hinder the recruitment, retention and advancement of Black medical students, residents and practitioners.
It is important to note the role of historically Black colleges and universities (HBCUs), which have represented an important piece in the pipeline. Nearly three-quarters – 70% – of all Black physicians in the U.S. attended HBCU medical schools.
At one time, there were seven HBCU medical schools. However, five of those seven were shuttered after the 1910 release of the Flexner Report, commissioned by Carnegie Corporation and the American Medical Association’s (AMA)’s Council on Medical Education. In 1910, Flexner published his report with devastating consequences for the numbers of Black doctors. He recommended shuttering five of the seven historically Black medical schools that trained the vast majority of Black physicians. Within two years of the Flexner Report, three Black medical schools closed, and by 1924, only two such schools remained.
Flexner claimed the Black medical schools were substandard. His biased thinking suggested that Black medical schools existed primarily to keep Black citizens from spreading contagious disease to the white population. The U.S. has yet to fully recover from this loss as there are now only four HBCU medical schools.
More critically, instead of providing assistance to help raise the quality of education at these schools, the AMA allowed them to close. Had they remained open, likely the number of Black physicians in this country today would be comparable to the size of the Black population, and more importantly, the tragic health disparities I’ve described would be much less.
HERE ARE SOME STEPS THAT NMA BELIEVES MUST BE TAKEN TO BEGIN TO ADDRESS THE SHORTAGE OF BLACK PHYSICIANS.
- Address barriers and inequities in the education system that prevent talented Black students from getting to medical schools, beginning with early childhood, through elementary and secondary school and pre-medical education at the undergraduate level.
- Black, Hispanic and Native American students are more likely to have parents without a college degree and more likely to attend a low-resourced college.
- Not only does that affect their ability to compete in the admissions process … these factors trickle down to social networks, limiting opportunities that affect their ability to succeed as medical students.
- For example, one study found that students of color were less likely to have shadowed a physician — an experience that can burnish a med school application.
- Pathway programs should offer early interventions and exposure to medical disciplines.
- Address financial constraints through scholarship opportunities and additional funding for low-income students. A student who is the first in their family to attend college, or who works 20 hours a week to pay expenses while attending college, faces an uphill battle. It’s much more difficult for those students to earn the same GPA and MCAT scores as a student who doesn’t have those constraints. NMA has established a Million Dollar Scholarship Challenge to help address that need – but it’s just a start. The burden of student debt disproportionately affects Black physicians, further exacerbating existing socioeconomic disparities.
- Ensure that guidance counselors at the high school level, and pre-med advisors at the undergraduate level, encourage and support Black students who aspire to medical careers. Black students are more likely to face discouragement from advisers when applying to medical school compared to their white counterparts. Instead of discouragement, they need support and resources.
- Create a more holistic admission process for medical school. Medical schools must expand their recruitment targets to include “added values” that underrepresented and racially minoritized individuals can bring to a training program or a department. Admission tests and grades don’t tell the whole story. To quote the American Medical Association (AMA) – “Scoring highly on the Medical College Admissions Test (MCAT)—one of the primary measurements used in consideration of medical student admission by medical schools—doesn’t mean you’ll become a great, or even a good, doctor.” The AMA report adds: “Overreliance on just one measure of performance, such as the MCAT, risks missing a pool of candidates with other valuable attributes to contribute to the health care system.” Aspiring Black medical school candidates have valuable attributes to contribute. They relate to Black patients and they contribute to better health outcomes. An admission process that overlooks that potential could exclude some of our best future doctors.
- Increase the number of residency positions.
- Address the issue of higher attrition rates among Black medical students and residents. These are students who managed to overcome barriers to get into medical school and on to residency. We need to understand what’s keeping them from meeting these final hurdles and how we can better support them.
- Address the especially severe shortage of Black men in medicine through continued support of funding for graduate medical education. Black men make up less than 3% of the overall physician population. This disturbing numbers stems from a history economic disadvantages and systemic racism.
- Continue and enhance programs in medical schools aimed at improving diversity. We’ve seen a backlash of late against DEI programs in medical schools. We cannot repeat the mistakes of the Flexner report. As HBCUs produce 70% of Black doctors, it is paramount that we continue to support these institutions and support increases in graduate medical education funding.
CLOSING COMMENTS
I believe we are at a turning point. In our lifetime, we have experienced two major life events that have significantly exposed the disparities between the health of Black people compared to those of our white counterparts: the COVID-19 pandemic and Hurricane Katrina. Both catastrophic events revealed the glaring health inequities that are present in our country. I believe we have the awareness and the political will to begin to create change.
As I said before, this is more than a matter of equity. It’s not just about representation and fairness. It’s about life and death. It’s about the health of millions of Black Americans.
There is much work to do, but there is also an opportunity to change the story.